OBJECTIVE: To evaluate current trends aimed to optimize healthy singleton term births, as defined by the Centers for Disease Control/ART reporting and assess the role blastocyst (BL) vitrification and preimplantation genetic screening (PGS) has played in our clinical management goal of “one embryo-one baby.” Additionally, we have critically weighed the pros and cons of routinely implementing these ART procedures in laboratory practice management.
DESIGN: Retrospective analysis of national CDC report summaries were compared to our clinical programs progressively applying freeze-all IVF cycles in conjunction with PGS in recent years. By contrasting industry trends regarding fresh donor egg (DE)-ET (control group) to autologous frozen ET cycles, we intuitively assessed practice gaps in number of embryos transferred, implantation rate and live birth rate (LBR)/ET, and showed how our clinical practices have improved the overall quality of patient care.
MATERIALS AND METHODS: Our routine laboratory procedures involve: ICSI, group culture in Global™ medium + protein supplement, tri-gas incubation, transvaginal ultrasound-guided ET, and the vitrification of BL using a microSecure/non-DMSO I.C.E. solution approach, with or without BL-biopsy/PGS.
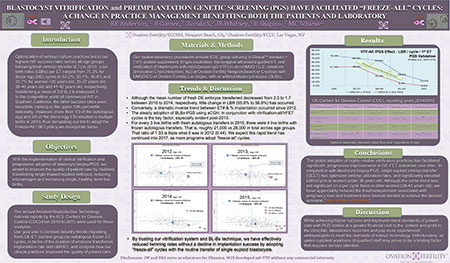
RESULTS: The mean number of fresh DE embryos transferred decreased from 2.0 to 1.7 between 2010 to 2014, with little change in LBR from 55.8% to 56.8%. Conversely, a similar annual trend transferring thawed DE-BL exhibited higher LBRs (34.9% to 41.5%, respectively). With emphasis on PGS in 2014, an affiliate clinic transferred 1.1 to 1.2 BL/ET in women <35 yo, 35-37yo, 38-40yo and 41-42yo (n>250 cycles), achieving implantation rates of 77.9%, 61%, 60% and 84%, respectively, and 71%, 69.4%, 71.4% and 64.3% in 2015 (per CDC). Transferring 1.1 BL/ET in women 41-42 yo (2014), resulted in a healthy, singleton term LBR of 69.6%, which was the highest value reported, as a percentage, for any age group or cycle type at any US center by the CDC in 2014.
CONCLUSIONS: BL biopsy practices have enhanced the efficacy of embryo use and cryostorage. Although there is more patient costs involved in single euploid ET cycles, the potential benefits include: reduced risk of miscarriages, decreased treatment intervals to term births, more singleton term births, and the avoidance of high neonatal costs asoociated with multiple births. Overall, our moral standards in patient care are aimed to improve healthy singleton LBRs. While achieving the latter phenomenon comes at a greater financial cost to the patient, and profit to the clinic/lab, laboratories are having to pay and hire more experienced Embryologists to meet the demands of todays’ technology. Unfortunately, an under-supplied skilled workforce of senior Embryologists may prove to be a limiting factor that requires serious attention.