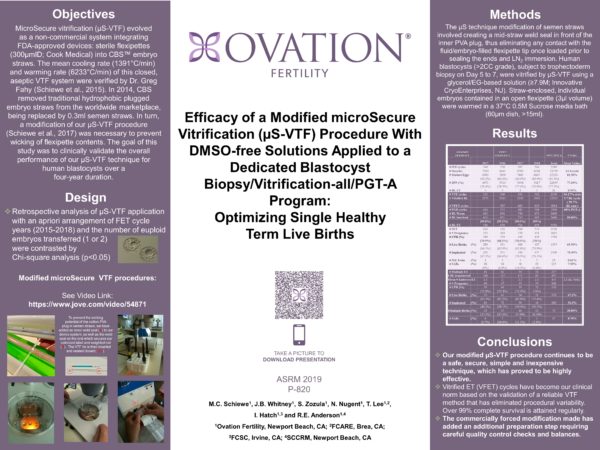
OBJECTIVE: MicroSecure vitrification (µS-VTF) evolved as a non-commercial, FDA-compliant device integrating sterile flexipettes (300µmID; Cook Medical) into CBS™ embryo straws. The mean cooling rate (1391°C/min) and warming rate (6233°C/min) of this closed, aseptic VTF system were verified by Dr. Greg Fahy (Schiewe et al., 2015). In 2014, CBS removed traditional hydrophobic plugged embryo straws from the worldwide marketplace, being replaced by 0.3ml semen straws. In turn, a modification of our µS-VTF procedure (Schiewe et al., 2017) was necessary to prevent wicking of flexipette contents. The goal of this study was to clinically validate the overall performance of our µS-VTF technique for human blastocysts over a 4-year duration.
DESIGN: Retrospective analysis of µS-VTF application with an apriori arrangement of FET cycle years (2015-2018) and the number of euploid embryos transferred (1 or 2) were contrasted by Chi-square analysis (p<0.05).
MATERIALS AND METHODS: The µS technique modification of semen straws involved creating a mid-straw weld seal in front of the inner PVA plug, thus eliminating any contact with the fluid-embryo filled flexipette tip once loaded prior to sealing the ends closed and LN2 immersion. Human blastocysts (>2CC grade) subject to trophectoderm biopsy on Day 5 to 7, were vitrified by µS-VTF using a Glycerol/EG-based solution (≥7.9M; Innovative CryoEnterprises, NJ). Straw enclosed, individual embryos contained in an open flexipette (3µl volume) were warmed in a 37°C 0.5M Sucrose media bath (60µm dish, >15ml). Following a 4-step dilution and 1-4h of tri-gas in vitro culture (37°C), ET was performed by transvaginal ultrasound guidance.
RESULTS: Between 2015-2018, 12,583 blastocysts were vitrified in 2,139 of 2,289 IVF patient cycles (94.2%; mean=5.7 blastocysts/cycle; mean patient age=37 years old). Of 2660 blastocysts warmed, 2640 survived completely (99%), as revealed by their cellular responsiveness to osmotic changes and intact membrane/cellular integrity. When single (n=2130) or multiple (n=237; mean=2.1 embryos/ET) vitrified-warmed ET was performed, 1500 (70.4%) and 260 (52.3%) blastocysts implanted, respectively. These implantation rates were different (p<0.05), eventhough ongoing/live birth rates were similar (65.5% versus 67.1%, respectively). Overall, vitrified embryo efficiency was significantly improved transferring a single euploid blastocyst, independent of patient age, having a monozygotic twinning rate of 0.61% in contrast to a potentially unhealthy 38.8% multiple birth rate transplanting ≥2 euploid embryos.
CONCLUSIONS: Since 2014, our clinical practice has predominantly (>85%) applied blastocyst biopsying/preimplantation genetic testing for aneuploidy (PGT-A) and >99% VTF-all cycles. Vitrified embryo transfer cycles have become our clinical norm. In turn, µS-VTF using non-DMSO, glycerol based solutions has been associated with some of the highest % healthy single term live birth rate as reported by the annual CDC/ART Surveillance survey (2014-2017). µS-VTF has continued to be safe, secure, simple and inexpensive technique.