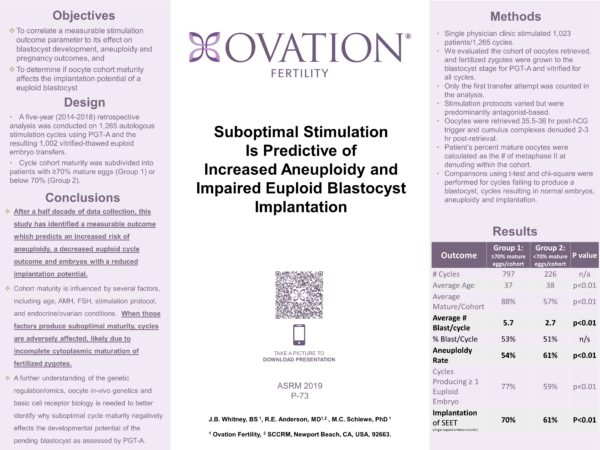
OBJECTIVE: To correlate a measurable stimulation outcome parameter to its effect on blastocyst (BL) development, aneuploidy and pregnancy outcomes, and determine if oocyte cohort maturity effects the implantation potential of a euploid BL.
DESIGN: Oocyte quality is difficult to independently quantify, while the percent of metaphase II (i.e., mature) oocytes within a cohort of cumulus oocyte complexes (COC) retrieved can be used to assess overall stimulation effectiveness. A 5-year (2014-2018) retrospective analysis was conducted on 1264 autologous cycles using PGT-A and 796 vitrified-warmed euploid BL transfers. Cycle cohort maturity was subdivided into patients with ≥70% mature eggs (Group 1) or <70% (Group 2).
MATERIALS AND METHODS: Single physician clinic stimulated 1046 patients for 1264 cycles. Oocyte maturity was evaluated, and all fertilized zygotes were grown to BL for biopsy/PGT-A and vitrification all cycles. Only first transfer attempts were compared in the per cycle analysis. Stimulation protocols were predominantly antagonist based. Oocytes were retrieved 35.5h post-hCG trigger, COC denuded 2-3h post-retrieval before ICSI and the % mature oocytes calculated. Comparisons using t-test and chi-square were performed for cycles failing to produce a BL, cycles resulting normal embryos, aneuploidy and implantation.
RESULTS: Average patient age was 37 and 38 years old for Groups 1 and 2, respectively (p<0.01), with a mean maturation rate of 88% and 57%. Oocyte maturity ≥70% (Group 1) occurred in 1038 cycles, while 226 cycles (18%) were identified as having suboptimal cohort maturity (Group 2). Group 2 had a reduced (p<0.01) mean BL yield of 2.4 blastocysts per cycle compared to 5.2 per Group 1 cycle. Yet, % BL production per cycle was not significant. Group 2 BL had a higher (p<0.01) aneuploidy rate (63 vs 56%) and more cycles failed to yield a normal embryo (52 vs 33%). Implantation of euploid BL derived from either group was not statistically different averaging 77%. While our overall live birth rate, independent of age, exceed 65% per euploid ET, the overall clinical pregnancy rate per cycle start was lower for Group 2 (35%) than Group 1 (52%).
CONCLUSIONS: It is well understood that multiple factors influence stimulation and oocyte maturity. Nonetheless, after a half decade of data collection, this study has identified a measurable outcome, oocyte cohort maturity, which predicts an increased risk of aneuploidy, a decreased euploid cycle outcome and embryos with a reduced implantation potential. Cohort maturity is influenced by several factors, including age, AMH, FSH, stimulation protocol, and endocrine/ovarian conditions. When those factors produce suboptimal maturity, cycles are adversely affected, likely due to incomplete cytoplasmic maturation of fertilized zygotes. A further understanding of the genetic regulation/omics, oocyte in-vivo genetics and basic cell receptor biology is needed to better identify why suboptimal cycle maturity negatively effects the developmental potential of the pending BL as assessed by PGT-A.